 |
| MMWR Weekly Vol. 65, No. 41 October 21, 2016 |
| PDF of this issue |
Notes from the Field: Outbreak of Zika Virus Disease — American Samoa, 2016
Weekly / October 21, 2016 / 65(41);1146–1147
Jessica M. Healy, PhD1,2,3; M. Catherine Burgess, MS4; Tai-Ho Chen, MD3; W. Thane Hancock, MD4; Karrie-Ann E. Toews, MPH4; Magele Scott Anesi, MPH5; Ray T. Tulafono Jr6; Mary Aseta Mataia5; Benjamin Sili5; Jacqueline Solaita5; A Christian Whelen, PhD7; Rebecca Sciulli, MSc7; Remedios B. Gose, MSPH7; Vasiti Uluiviti, MSc8; Morgan Hennessey, DVM1,9; Fara Utu5; Motusa Tuileama Nua5; Marc Fischer, MD9 (View author affiliations)
View suggested citationDuring December 2015–January 2016, the American Samoa Department of Health (ASDoH) detected through surveillance an increase in the number of cases of acute febrile rash illness. Concurrently, a case of laboratory-confirmed Zika virus infection, a mosquito-borne flavivirus infection documented to cause microcephaly and other severe brain defects in some infants born to women infected during pregnancy (1,2) was reported in a traveler returning to New Zealand from American Samoa. In the absence of local laboratory capacity to test for Zika virus, ASDoH initiated arboviral disease control measures, including public education and vector source reduction campaigns. On February 1, CDC staff members were deployed to American Samoa to assist ASDoH with testing and surveillance efforts.
To track the progression of the outbreak in the absence of confirmed case results, trends in the number of suspected Zika virus disease cases were monitored through syndromic surveillance using automated searches of the electronic health record (EHR) system at the one hospital and four health care clinics in the territory. Suspected cases were identified among persons having ≥1 admission diagnosis of “Zika,” “dengue,” “chikungunya,” “viral exanthem,” “acute fever,” or “rash.” During January–July 2016, among a total population of 55,502 persons, 756 suspected cases were identified for an overall incidence of 13.6 per 1,000 persons. The incidence of suspected cases was highest (18.4 per 1,000) in Ituau County (population = 4,676).
To establish laboratory capabilities, ASDoH collaborated with the Pacific Island Health Officer Association, the Hawaii Department of Health, and CDC. During January–July 2016, serum specimens were collected from 98 pregnant women who had sought testing, regardless of their symptoms, as well as from 90 nonpregnant female and male patients within 5 days of at least one sign or symptom of Zika virus disease, including fever, rash, arthralgia, or conjunctivitis. Weekly shipments of two to 25 specimens (median = eight specimens per week) were sent to the Hawaii Department of Health laboratory for testing and to CDC’s Arboviral Diseases Branch for confirmatory testing; among the 188 specimens collected, two were damaged during shipping and could not be tested. Fifty-one (27%) of the 186 specimens tested had evidence of recent Zika virus infection by real-time, reverse transcription–polymerase chain reaction (rRT-PCR) (n = 25) or by sequential testing using immunoglobulin M antibody capture enzyme-linked immunosorbent assay (MAC-ELISA) and neutralizing antibody titers against Zika virus that were ≥fourfold higher than titers against dengue virus (n = 26) (3).
Among the 98 pregnant women who were tested, 19 (19%) had laboratory evidence of recent Zika virus infection, including 18 of 70 (26%) symptomatic women and one of 28 (4%) asymptomatic woman. One case of dengue virus infection was identified by MAC-ELISA and neutralizing antibody testing; no cases of chikungunya were identified. The overall incidence of confirmed Zika virus infection was 0.92 per 1,000 persons and was highest (2.77 per 1,000) in Leasina County (population = 1,807). The weekly number of both suspected infections identified through syndromic surveillance and confirmed infections peaked during January 24–30; the month with the highest number of confirmed cases was February (Figure). In any week, there were four to 34 (median = 11) times as many suspected cases as confirmed cases identified.
A registry of all currently pregnant women identified in the territory was created to facilitate monitoring for adverse outcomes and implementing targeted prevention efforts. Pregnancies beginning as early as May 2015 were identified through EHR searches, and newly identified pregnancies were reported by the four prenatal clinics on the island. Data from 674 women were entered in the registry, including all 98 pregnant women who were tested. Initial medical record review indicated that the majority of pregnant women who sought prenatal care did so during their third trimester of pregnancy. To encourage women to seek earlier prenatal care, public messaging and clinic fee waivers were implemented. To reduce the risk of Zika virus transmission, prenatal health clinics distributed Zika prevention kits containing mosquito repellents, bed nets, and condoms to 674 pregnant women.
This report details the introduction of Zika virus into American Samoa and the challenges presented during the response. Off-island testing by the Hawaii Department of Health and CDC facilitated identification of 51 confirmed Zika virus infections. Because of delays inherent in off-island testing, the existing ASDoH EHR system was used to identify suspected cases for outbreak tracking, and to identify pregnancies for monitoring. The trend in suspected cases approximated the trend in confirmed cases over time, but not by county. Collaboration among multiple public health agencies helped to mitigate these challenges and highlights the importance of continued strengthening and coordination of epidemiologic and laboratory capacity in the Pacific Islands.
Corresponding author: Jessica M. Healy, jhealy@cdc.gov, 619-692-5571.
1Epidemic Intelligence Service, CDC; 2Epidemiology and Immunization Services Branch, County of San Diego Health and Human Services Agency, San Diego, California; 3Division of Global Migration and Quarantine, National Center for Emerging and Zoonotic Infectious Diseases, CDC; 4Division of State and Local Readiness, Office of Public Health Preparedness and Response, CDC; 5Department of Health, American Samoa Government; 6Lyndon B. Johnson Tropical Medical Center, American Samoa; 7Hawaii Department of Health State Laboratories Division; 8Pacific Islands Health Officer’s Association, Honolulu, Hawaii; 9Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases, CDC.
References
- Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects—reviewing the evidence for causality. N Engl J Med 2016;374:1981–7. CrossRef PubMed
- Broutet N, Krauer F, Riesen M, et al. Zika virus as a cause of neurologic disorders. N Engl J Med 2016;374:1506–9. CrossRef PubMed
- CDC. Zika virus disease and Zika virus infection, 2016 case definition. Atlanta, GA: CDC; 2016. https://wwwn.cdc.gov/nndss/conditions/zika-virus-disease-and-zika-virus-congenital-infection/case-definition/2016/
 FIGURE. Number of laboratory-confirmed* cases of Zika virus infection in pregnant women (n = 19) and the general population (n = 32), and number of suspected cases derived from electronic health record (EHR) searches (n = 756), by month of onset — American Samoa, January 3–July 16, 2016
FIGURE. Number of laboratory-confirmed* cases of Zika virus infection in pregnant women (n = 19) and the general population (n = 32), and number of suspected cases derived from electronic health record (EHR) searches (n = 756), by month of onset — American Samoa, January 3–July 16, 2016
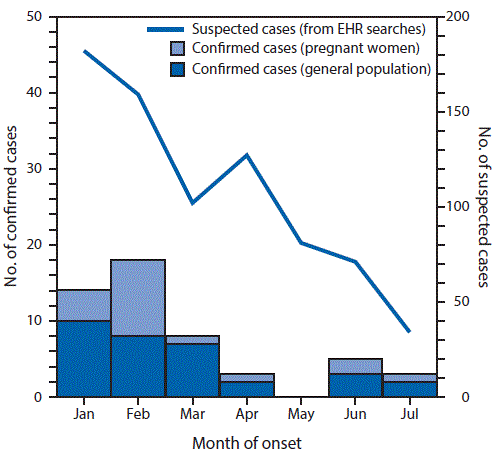
* By real-time reverse transcription–polymerase chain reaction or serology.


































No hay comentarios:
Publicar un comentario