
Combination Therapy Improves Survival for Some Men with Recurrent Prostate Cancer
February 13, 2017, by NCI Staff
Adding androgen deprivation therapy to radiation therapy can improve survival for some men with recurrent prostate cancer, according to the long-term results of a clinical trial.
The combination therapy was also associated with a lower rate of metastases and death due to prostate cancer, compared with radiation alone. William U. Shipley, M.D., of Massachusetts General Hospital and his colleagues reported their findings in the New England Journal of Medicine on February 2.
The NCI-sponsored clinical trial included 760 patients who had undergone surgery to remove the prostate as treatment for localized cancer and later experienced rising prostate-specific antigen(PSA) levels, a change known as a biochemical recurrence that may indicate that the disease has returned.
"Surgery is a very common treatment for men with localized prostate cancer, but more than 30% of them will have recurrent disease,” Dr. Shipley noted in a news release. He predicted that the study results would change the standard of care for patients who experience a postoperative recurrence.
Study Results
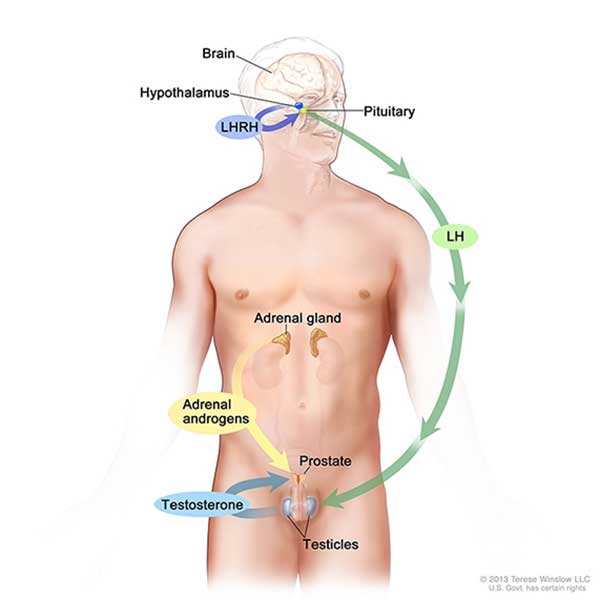
In the trial, participants were randomly assigned to receive bicalutamide (Casodex®) or a placebo for 24 months, along with 6.5 weeks of radiation therapy. When the trial began in 1998, bicalutamide was a commonly used treatment to prevent androgens (male sex hormones) from fueling the growth and spread of tumors in men with prostate cancer.
The patients were followed for a median of 13 years. The overall survival rate among patients in the bicalutamide group at 12 years was 76.3%, compared with 71.3% in the placebo group—a statistically significant difference.
By 12 years, 21 (5.8%) of the patients receiving bicalutamide had died from prostate cancer, versus 46 (13.4%) patients in the placebo group, the researchers found. In the bicalutamide group, 14.5% of the patients developed distant metastases by 12 years, versus 23.0% of those in the placebo group.
The main side effect of bicalutamide was the growth of breast tissue, or gynecomastia, which was seen in nearly 70% of the men who received this drug and 11% of those in the placebo group.
This side effect can be “distressing,” but it can be “mitigated by prophylactic radiation of the breast or by the administration of tamoxifen,” wrote Ian M. Thompson, Jr., M.D., of CHRISTUS Santa Rosa Health System, in San Antonio, Texas, in an accompanying editorial.
The rate of long-term side effects, including effects on the heart and liver, were not statistically significantly different between the groups. Therapies that interfere with the production or the action of the androgen testosterone have been linked to these effects in previous studies.
Growing Body of Evidence
The results are consistent with those of a clinical trial published last year that tested the addition of short-term androgen deprivation therapy to radiation therapy, noted Deborah E. Citrin, M.D., of NCI’s Center for Cancer Research (CCR), who was not involved in either study. The findings of the 2016 trial indicated that radiation plus a course of androgen deprivation therapy for 6 months could be a treatment option for men who experience a biochemical recurrence after a prostatectomy.
“Together, the results of these studies give us much more confidence in recommending this type of treatment for the appropriate patients,” said Dr. Citrin, a senior investigator in CCR’s Radiation Oncology Branch.
“Now that we know there’s a survival benefit, we need to determine who is likely to benefit most from the treatment and what the optimal duration of treatment is,” Dr. Citrin continued. Some patients may achieve some of the benefits reported in the bicalutamide trial from shorter courses of androgen deprivation therapy, she noted.
Patients considering treatment with androgen deprivation therapy and radiation therapy should discuss the option with their doctors “to find a balance between the potential benefits and the risks, including side effects,” Dr. Citrin added.
In recent years, drugs such as leuprolide acetate (Lupron®) have largely replaced bicalutamide as an adjunct to radiation. Two major clinical trials that began about 5 years ago are testing some of these agents in combination with radiation.
“It will take some time to get their results,” Dr. Shipley noted. But since both approaches act by lowering the supply of testosterone to the tumor itself, there isn't any reason to expect the results to be different from the bicalutamide trials, he added.
Value of Long-Term Follow-Up
In 2010, interim results of the current study showed that treatment with bicalutamide led to a reduction in both biochemical recurrence and the development of metastases. Because prostate cancer can progress slowly, the researchers wanted longer-term follow-up to determine whether some participants could be considered cured of their disease.
In his editorial, Dr. Thompson highlighted this aspect of the research.
“This remarkable contribution by the National Clinical Trials Network of the National Cancer Institute shows the importance of randomized clinical trials with very long follow-up,” he wrote. “Studies that incorporate interventions without proprietary intellectual property (e.g., surgery or radiation therapy) or pharmaceutical agents whose patents often expire before the study is completed can be achieved only with the use of this invaluable national resource.”


































No hay comentarios:
Publicar un comentario