Continued CDC Funding for States to Detect, Respond, Prevent and Innovate
Through CDC’s Epidemiology and Laboratory Capacity for Infectious Diseases (ELC) Cooperative Agreement, CDC continues to work with state and local health departments to implement tracking, prevention, and antibiotic stewardship activities – transforming how the nation combats and slows antibiotic resistance at all levels.
In addition to investments made last year, CDC is inviting grantees to participate in enhanced activities, potentially including:
- Whole genome sequencing in all states to determine AR profiles for every Salmonella isolate, and expanding testing for other germs in the future.
- Enhanced epidemiologic support for foodborne investigations—interviewing more patients faster and in greater detail—to ensure rapid response.
- Identifying new ways to prevent human infection caused by resistant bacteria in food animals, through NARMS and partnerships with FDA and USDA.
- Increased testing nationwide for the fungal threat Candida, including C. auris.
- Using Integrated Food Safety Centers of Excellence to provide instructional materials on antimicrobial resistance for veterinarians.
These activities will enhance capacities to rapidly detect antibiotic resistance and prevent its spread to better protect Americans. Visit CDC’s antibiotic resistance website for the funding announcement.
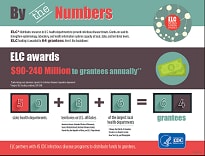
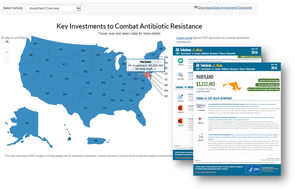 See how CDC invested in every state in 2016 to combat antibiotic resistance in healthcare facilities, the community, and food. Local CDC investments through ELC combat antibiotic resistance by strengthening the public health workforce and building stronger surveillance systems, modern and efficient laboratory facilities, and more integrated health information networks. Epidemiology and Laboratory Capacity for Infectious Diseases (ELC) Cooperative AgreementGranteesCDC’s Epidemiology and Laboratory Capacity for Infectious Diseases Cooperative Agreement (ELC) funds all 50 state health departments, six of the nation’s largest local health departments (Chicago, the District of Columbia, Houston, Los Angeles County, New York City and Philadelphia), and eight territories or U.S. affiliates, including U.S. Virgin Islands, Puerto Rico and Guam. There are 64 grantees. Public Health ImpactAs Americans are increasingly affected by infections emerging anywhere in the world, finding and stopping infectious disease health threats is essential to protecting public health and saving lives. Communities across the nation benefit from the actions taken by state, local, and territorial public health departments to detect, respond, prevent, and control known and emerging (or re-emerging) infectious diseases. Examples of other benefits:
Grantee ActivitiesState, local, and territorial public health agencies each have unique needs and priorities because of the diverse infectious disease challenges they face, their organizational capacity, geography, and populations. Often, there are unanticipated events that may require the diversion of resources to a specific emerging or re-emerging disease. To better meet essential needs and reduce delays in responsiveness, cross-cutting ELC resources are designed to address planned-for and unanticipated infectious disease threats. The ELC oversees an array of projects that strengthen the ability of public health agencies to respond to, prevent, and control known and emerging (or re-emerging) infectious diseases. These include the growing threat of drug-resistant infections , foodborne disease prevention and tracking , vaccine-preventable diseases , as well as activities to reduce healthcare-associated infections.Two primary classes of ELC funding include: Flexible or Non-disease-specific fundingtackles high-priority needs that are NOT disease-specific. Funding in this category addresses integrated, cross-cutting activities related to epidemiology, laboratory, and health information systems. Resources are awarded so grantees can: |























.png)











No hay comentarios:
Publicar un comentario