Antifungal Resistance
Fungal infections that are resistant to treatment are an emerging public health problem, but everyone has a role in preventing these infections and reducing antifungal resistance.Just like antibiotics cure bacterial infections, antifungal medications save lives by curing dangerous fungal infections. And just like some bacterial infections are resistant to antibiotics, some fungi no longer respond to the antifungal medications that are designed to cure them. This emerging phenomenon is known as antifungal resistance, and it’s primarily a concern for invasive infections with the fungus Candida.
Although antibiotic-resistant bacterial infections are a widely-recognized public health threat, less is known about the effects of antifungal resistance and the burden of drug-resistant fungal infections. This highlights the need for an improved understanding of the reasons for their emergence, heightened awareness among medical and public health communities about these infections, and greater attention to methods that can be used to prevent and control them.
The problem
Invasive fungal infections cause substantial morbidity and mortality and are a costly, common problem in healthcare settings. The fungus Candida is the most common cause of healthcare-associated bloodstream infections in the United States.1 Each case of Candida bloodstream infection (also known as candidemia) is estimated to result in an additional 3 to 13 days of hospitalization and $6,000 to $29,000 in healthcare costs.2
What’s also concerning is that some types of Candida are becoming increasingly resistant to first-line and second-line antifungal medications, namely, fluconazole and echinocandins (anidulafungin, caspofungin, and micafungin). Approximately 7% of all Candida bloodstream isolates tested at CDC are resistant to fluconazole, most of which are Candida glabrata.3,4 CDC’s surveillance data indicate that the proportion of Candida isolates that are resistant to fluconazole has remained fairly constant over the past twenty years.4–6 Echinocandin resistance, however, appears to be on the rise, especially among Candida glabrata. CDC’s surveillance data indicate that up to 8% of Candida glabrata isolates in 2014 may not be susceptible to echinocandins; this proportion nearly doubled from 4% in 2008. This is especially concerning as echinocandins are the mainstay of treatment for Candida glabrata, which already has high levels of resistance to fluconazole.3
What’s also concerning is that some types of Candida are becoming increasingly resistant to first-line and second-line antifungal medications, namely, fluconazole and echinocandins (anidulafungin, caspofungin, and micafungin). Approximately 7% of all Candida bloodstream isolates tested at CDC are resistant to fluconazole, most of which are Candida glabrata.3,4 CDC’s surveillance data indicate that the proportion of Candida isolates that are resistant to fluconazole has remained fairly constant over the past twenty years.4–6 Echinocandin resistance, however, appears to be on the rise, especially among Candida glabrata. CDC’s surveillance data indicate that up to 8% of Candida glabrata isolates in 2014 may not be susceptible to echinocandins; this proportion nearly doubled from 4% in 2008. This is especially concerning as echinocandins are the mainstay of treatment for Candida glabrata, which already has high levels of resistance to fluconazole.3
The stable yet substantial rates of fluconazole resistance and the emergence of echinocandin resistance are concerning because echinocandins are typically used to treat infections caused by C. glabrata, the species that’s most often associated with fluconazole resistance. For multi-drug resistant Candida infections (those that are resistant to both fluconazole and an echinocandin), the few remaining treatment options are expensive and can be toxic for patients who are already very sick. Not surprisingly, there is growing evidence to suggest that patients who have drug-resistant candidemia have poorer outcomes than patients who have candidemia that’s susceptible to antifungal medications.7,8 Overall, antifungal resistance is still relatively uncommon, but the problem will likely continue to evolve unless more is done to prevent further resistance from developing and prevent the spread of these infections.
The cause
Some species of fungi are naturally resistant to certain types of antifungal medications. Other species may be normally susceptible to a particular type of medication, but develop resistance over time as a result of improper antifungal use—for example, dosages that are too low or treatment courses that aren’t long enough.9,10 Some studies have indicated that antibacterial medications may also contribute to antifungal resistance; this could occur for a variety of reasons, one of which is that antibacterials reduce bacteria in the gut and create favorable conditions for Candida growth.11 It’s not yet known if decreasing the use of all or certain antimicrobial agents can reduce Candida infections, but appropriate use of antibacterial and antifungal agents is one of the most important factors in fighting drug resistance.
It’s not just Candida
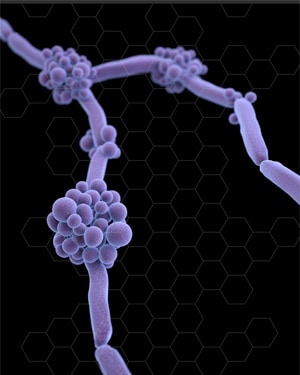
Microscopic view of Aspergillus
Although most antifungal resistance occurs in Candida species, resistance in other types of fungi, such as Aspergillus, is also an emerging issue. The full extent of the problem is still unknown, but the global prevalence of azole resistance in Aspergillus is estimated to be approximately 3 to 6 percent.12
As with Candida, Aspergillus infections are associated with high mortality, and resistant infections can develop in people who’ve had previous exposure to certain antifungal medications.13 In addition, some studies suggest that resistance in Aspergillus may be partially driven by the use of agricultural azoles, which protect crops from fungi.14, 15 More research is needed about the mechanisms of resistance in Aspergillus and the prevention of resistant Aspergillus infections.
What can be done
Antifungal resistance is becoming increasingly recognized, particularly for Candida. Everyone has a role in preventing Candida infections and reducing antifungal resistance.
- CDC is:
- Tracking trends in antifungal resistance through the Emerging Infections Program by conducting multi-center candidemia surveillance and performing species confirmation and antifungal susceptibility testing on Candida bloodstream isolates.3,4
- Using genetic sequencing and developing new laboratory tests to identify and understand specific mutations associated with antifungal resistance in Candida.
- Hospital executives and infection control staff can:
- Assess antifungal use as part of their antibiotic stewardship programs.
- Ensure adherence to guidelines for hand hygiene, prevention of catheter-associated infections, and environmental infection control.
- Doctors and other hospital staff can:
- Prescribe antifungal medications appropriately.
- Document the dose, duration, and indication for every antifungal prescription.
- Stay aware of local antifungal resistance patterns.
- Participate in and lead efforts within your hospital to improve antifungal prescribing practices.
- Follow hand hygiene and other infection control measures with every patient.
- Hospital patients can:
- Be sure everyone cleans their hands before entering your room.
- If you have a catheter, ask each day if it is necessary.






















.png)











No hay comentarios:
Publicar un comentario