
Immune ‘hotspots’ could help predict the risk of breast cancer relapse in patients, study finds
Scientists from The Institute of Cancer Research, London has developed a new test through which women at a greater risk of relapsing from breast cancer within 10 years of diagnosis can be identified.
In the study, published today in the Journal of the National Cancer Institute, the researchers used immune cell ‘hotspots’ in and around the tumors able to predict a women’s likelihood of breast cancer relapse. They found that women who possessed a large number of hotspots were more prone to relapse when compared with women who had less hotspots.
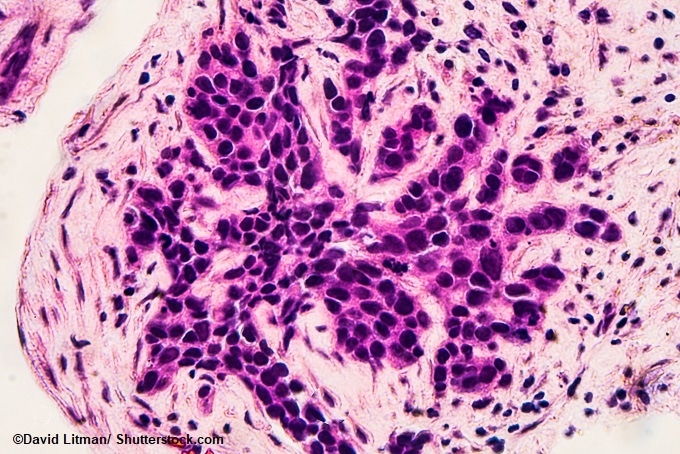
Image: Photomicrograph of core biopsy for infiltrating (invasive) ductal carcinoma, detected by screening mammogram. H & E stain.
This new test is expected to aid in the more accurate assessment of the risk of reoccurring cancer in individual patients and help in offering them monitoring or preventive treatments.
Tissue samples from 1,178 women who were affected with estrogen receptor positive breast cancer – the most common type of breast cancer –were analyzed in the study. These samples were obtained as a part of a clinical trial done at The Royal Marsden NHS Foundation Trust that compared two hormone therapies which has the capability to prevent cancer from relapsing after the surgery. In order to analyze these samples, the team developed a new, completely automated computer tool.
The results showed that, in comparison with the immune cells that are equally dispersed in the hotspots, the chance of recurrence within a period of 10 years from the start of the treatment was 25% higher when the immune cells were clustered together. Also, in women with immune cell hotspots, the chance of re-occurrence of the cancer within the duration of 5 years was 23% higher.
Prior research done by the team that focused at the tumor samples from estrogen receptor-negative breast cancer found an opposite effect; here, the clustering of the immune cells in the hotspots were associated with a less chance of relapse.
With the support of the Breast Cancer Now, Cancer Research UK and Wellcome, NIHR Biomedical Research Centre at The Royal Marsden NHS Foundation Trust and the ICR funded the study.
After the validation of the test, it is expected to aid predicting the risk of relapsing of the cancer as well as deciding the apt course of treatment.
The effect of immune hotspots on the possibility of recurrence can be associated to the mechanism of working of the immune system in these cancers.
Although Dr Yinyin Yuan, Team Leader in Computational Pathology at the ICR, expressed enthusiasm for a test that could be used to identify patients who have the highest risk of relapse in the future, larger studies must be carried out before the immune hotspot test can be implemented in the clinic. But huge benefits are to be seen if this became a reality, including ease and cost-effective advantages and even the possibility to develop a further test to evaluate a patients’ response to immunotherapy, prior to treatment.
Professor Mitch Dowsett, Head of the Ralph Lauren Centre for Breast Cancer Research at The Royal Marsden, and Professor of Endocrinology at the ICR said: “There are a number of molecular tests used in the management of women with early breast cancer but none of these have focused on the immune aspects of the disease.”
He expects that the findings of this study, in future, will help to improve the use of such tests, by which the improved management of over 40,000 women who develop this kind of breast cancer in the UK every year.
Professor Paul Workman, Chief Executive of the ICR, also commented that the development of the new computer based-test has the capability to automate analysis of breast cancer sample by differentiating different patterns, not possible to see under the microscope. He believes that the study reveals the possibility of the immune system to play a key role in the way breast cancer responds to the hormone treatment.






















.png)











No hay comentarios:
Publicar un comentario