
Creative Minds: Potential Diabetes Lessons from Binge-Eating Snakes
Many people would do just about anything to avoid an encounter with a snake. Not Stephen Secor. Growing up in central New York State, Secor was drawn to them. He’d spend hours frolicking through forest and field, flipping rocks and hoping to find one. His animal-loving mother encouraged him to keep looking, and she even let him keep a terrarium full of garter snakes in his bedroom. Their agreement: He must take good care of them—and please make sure they don’t get loose.
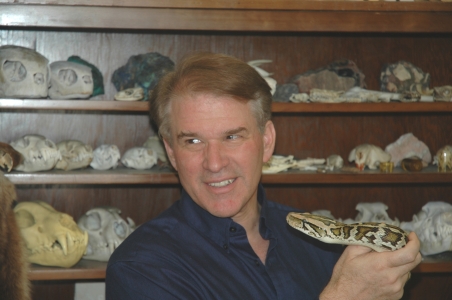
As a teen, Secor considered a career as a large-animal veterinarian. But a college zoology course led him right back to his fascination with snakes. Now a professor at the University of Alabama, Tuscaloosa, he’s spent 25 years trying to understand how some snakes, such as the Burmese python shown above, can fast for weeks or even months, and then go on a sudden food binge. Secor’s interest in the feast-or-famine digestive abilities of these snakes has now taken an unexpected turn that he never saw coming: a potential treatment to help people with diabetes.
Secor’s studies have shown that between meals, Burmese pythons, boa constrictors, sidewinder rattlesnakes, and other “infrequently feeding” snakes shut down many of their cells as an energy-saving measure. As a result, vital organs—including the small intestine, liver, kidneys, heart, and pancreas—begin to lose a lot of their capabilities. When those snakes break their fast, they must immediately get their organs back up and running to digest the meal and transport oxygen and nutrients throughout the body.
So how do they do it? In an earlier study, Secor’s team discovered that fatty acids in the blood of Burmese pythons after a large meal encourage healthy heart growth [1]. Intriguingly, he found a fatty-acid cocktail from these pythons, when delivered to mice, also encouraged heart growth.
With the support of an NIH Director’s 2016 Transformative Research Award, Secor and his co-investigators Amit Choudhary and Bridget Wagner at the Broad Institute of MIT and Harvard, Cambridge, MA, are in search of chemical compounds, or small molecules, in snake blood that might do similar things for the pancreas. They’re specifically interested in factors that help to restore its insulin-producing beta cells, which can be destroyed or damaged in people with diabetes.
The team is just getting started, but they’ve already seen in the lab that human beta cells incubated with the blood of fed snakes increase in size. Those cells also begin to produce more insulin and can withstand stressful conditions that are normally toxic to beta cells.
In search of small molecules responsible for those beneficial effects of snake blood, the Broad team is looking closely at the underlying changes in gene activity in treated versus untreated human beta cells. Meanwhile, Secor is going back to studies in his snakes. He’ll isolate pancreatic cells and blood samples from snake species that eat often and those that don’t, before shipping them off to the Broad for genetic analysis.
The hope is that understanding these processes in snakes might offer strategies to boost insulin production in people with diabetes by repairing or protecting beta cells. The genes and small molecules identified in the snakes could also prove to be promising targets or candidates for future anti-diabetes drugs.
Surprising as it may seem, lessons learned from snakes have the potential to help hundreds of millions of people with diabetes around the world. For most of us who tend to think of snakes as a rather frightful part of the animal kingdom, we might take a moment to consider that.
Reference:
[1] Fatty acids identified in the Burmese python promote beneficial cardiac growth. Riquelme CA, Magida JA, Harrison BC, Wall CE, Marr TG, Secor SM, Leinwand LA. Science. 2011 Oct 28;334(6055):528-31.
Links:
Secor Lab (University of Alabama, Tuscaloosa)
Choudhary Lab (Harvard Medical School, Boston, MA)
Wagner Group (Broad Institute, Cambridge, MA)
Project Information (NIH RePorter)
NIH Support: National Institute of Diabetes and Digestive and Kidney Diseases; Common Fund






















.png)











No hay comentarios:
Publicar un comentario