
TMIST Trial Aims to Provide Clarity on Breast Cancer Screening Approaches
October 30, 2017, by NCI Staff
A large nationwide clinical trial has been launched to try to answer some important questions about the technologies used to screen for breast cancer.
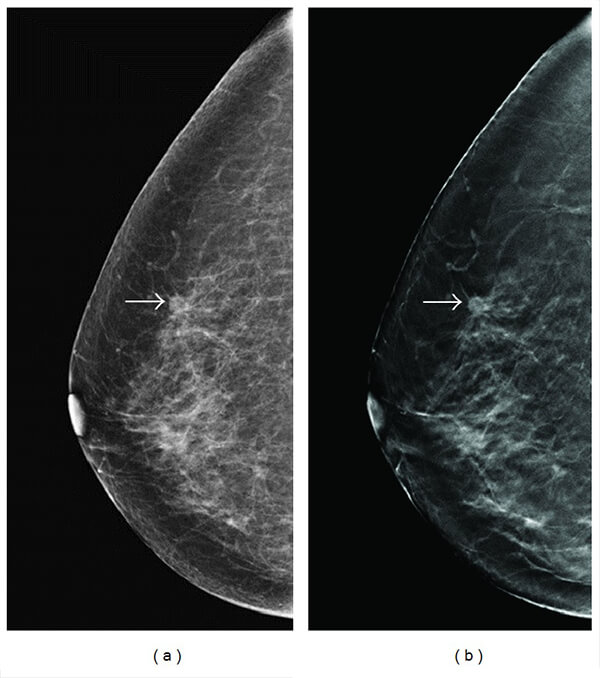
Known as the Tomosynthesis Mammographic Imaging Screening Trial, or TMIST, the NCI-funded trial is comparing two techniques used for mammograms: tomosynthesis, often called 3D mammography, and standard 2D digital mammography.
Over the past few weeks, the first participating centers have begun to enroll women in the trial. Eventually, approximately 100 sites in the United States and Canada are expected to participate, with a plan to enroll approximately 165,000 women between the ages of 45 and 74.
The trial is designed to resolve an important unknown: whether tomosynthesis has a meaningful impact on the detection of potentially life-threatening breast cancers, explained the study’s principal investigator, Etta Pisano, M.D., of Beth Israel Deaconess Medical Center in Boston and chief science officer of the American College of Radiology.
A key goal of TMIST, Dr. Pisano explained, is to help clinicians better understand the role of tomosynthesis in breast cancer screening.
“We know that we need to screen, period,” Dr. Pisano said. “The question is, are the newer tools really benefiting women as much as we hope they are.”
Head-to-Head Comparison of 2D and 3D Mammography
Led by the ECOG-ACRIN Cancer Research Group, TMIST will be the first large randomized clinical trial of screening mammography in decades. It will also be the first to directly compare the current standard technology for breast cancer screening, 2D digital mammography, against tomosynthesis.
The trials from the 1980s and 1990s that showed that regular screening with mammography could reduce the number of women who die from breast cancer used film mammography.
Digital mammography—meaning that the x-ray images are captured digitally and can be viewed more clearly on high-resolution computer screens—has largely overtaken film mammography over the past decade, said Martin Yaffe, Ph.D., of Sunnybrook Health Sciences Centre and the lead investigator for a TMIST “lead-in” trial that has been ongoing in Canada for nearly 3 years.
Although digital has several advantages over film mammography, Dr. Yaffe said, it still only produces flat two-dimensional images, akin to the moon’s flat appearance in the sky.
With tomosynthesis, on the other hand, images are captured all around the breast and are then assembled by a computer into a 3D-like image. Tomosynthesis is “not truly 3D, but close to it,” Dr. Yaffe explained.
The first tomosynthesis device for breast cancer screening was cleared by the Food and Drug Administration (FDA) in 2011. Of the machines currently used for screening mammography in the United States, 28% are tomosynthesis machines, a number that, according to FDA data, has remained flat for at least the last year.
The 3D technology has caught women’s interest, said Jennifer Simas, R.N., a clinical trials coordinator at Carson Tahoe Cancer Center in Nevada. TMIST is the first screening trial in which the center has participated.
Carson Tahoe—which screens between 150-200 women a day for breast cancer—started offering screening with tomosynthesis last year, and with that has come demand.
“A lot of women do want to be screened with the 3D [machine],” Simas said.
Dr. Pisano said she understands the allure of the newer technology. But, she continued, tomosynthesis does have some disadvantages compared with standard digital mammograms. The radiation dose with tomosynthesis, for example, can be more than two times what is received during standard digital mammography.
Dr. Yaffe explained that the higher radiation is due, in part, to the fact that tomosynthesis machines can perform standard 2D scans as well, and radiologists often do both the 2D and the 3D scans. Because tomosynthesis is still relatively new, he said, radiologists do this “partly out of caution.”
Tomosynthesis devices are also more expensive than standard digital mammography machines. And more time is required for the screening procedure and analysis, meaning that “it’s more expensive for patients and insurers,” Dr. Pisano said.
Simas confirmed that cost, for the moment at least, has been an issue for some women. Many women who ask to be screened using tomosynthesis don’t get it, she explained, “because their insurance won’t cover it.”
Nevertheless, with both technologies in regular use in centers across the country, Dr. Pisano said, a direct comparison was needed.
Finding Fewer Advanced Breast Cancers Over Time?
Once enrolled in TMIST, women will be randomly assigned to screening with either tomosynthesis or 2D digital mammography. Most women in the study will be screened once a year for 5 years.
However, women who are past menopause and who have none of the primary breast cancer risk factors (such as a family history of breast cancer or dense breasts) will be screened every other year for 5 years—meaning they will only undergo three rounds of screening, rather than five.
Studies have shown that these women have a generally lower risk for developing aggressive breast cancer, so the panel of experts who helped design TMIST concluded that these women could safely undergo less frequent screening, Dr. Pisano said.
The trial’s primary endpoint—the key question the study leaders hope to answer—is not how many women in each group die. Rather, the trial is designed to see whether tomosynthesis reduces the incidence of life-threatening breast cancers.
In many ways the endpoint is a matter of practicality, Dr. Pisano explained.
“We can’t do a mortality endpoint study,” she said. “It would take too long, 10 to 20 years.”
So reduction in the rate of advanced cancers—which are the most likely to be fatal—is, in effect, a surrogate for mortality.
“If one is a better screening tool than the other, there should be fewer advanced cancers [in that group] over 5 years of screening,” she said. Any breast tumors likely to cause harm “should have been found earlier, when they’re smaller, when they’re more easily treatable.”
Thus, the trial design should also help to answer the converse of this question, she added. Instead of detecting invasive cancers that could prove to be fatal, “are we finding too many things [with tomosynthesis] that won’t progress or that won’t kill women because they’re very slow-growing cancers?”
Answers Screening Questions and Maybe More
TMIST also has several important informational goals beyond its primary endpoint. These secondary endpoints include whether women screened with tomosynthesis have fewer call backs, or recalls, and biopsies for suspicious findings that eventually turn out not to be cancer—so-called false positives.
One hope with tomosynthesis is that the more complete view of the breast will reduce the rate of false-positive results compared with standard digital mammography, Dr. Pisano said. But data on whether that’s the case has so far been mixed, she cautioned.
“The trial should also help to identify whether screening with tomosynthesis increases the overdiagnosis of breast cancer and to what degree,” said Barry Kramer, M.D., M.P.H., director of NCI’s Division of Cancer Prevention. Overdiagnosis refers to the cancers that are diagnosed but that likely would never have caused any harm because they were too slow growing.
Other secondary endpoints include the rate of interval cancers—that is, breast cancers diagnosed in the interval between a prior negative mammogram and the next scheduled mammogram.
The TMIST findings, Dr. Yaffe said, will hopefully provide important information about how best to use these different screening technologies.
“For some women, we may find that a 2D digital mammogram is perfectly adequate,” he said. “It may be that some women should continue to get 2D digital mammograms while others should get tomosynthesis, depending on the characteristics of their breasts.”
The trial may very well help to answer other questions about the underlying biology of different forms of breast cancer, Dr. Pisano said. As part of the trial, a biorepository is being established to store tissue and blood samples from participants.
The biorepository, she continued, should produce a bona fide treasure trove for cancer researchers.
“It will be a great resource for future studies,” she said.
TMIST investigators, for example, already have ancillary studies planned to look at biomarkers in tissue and blood samples that correlate not only with breast cancer but other cancer types as well.
The size and scope of the trial should have other tangible benefits as well, said Bruce Rapkin, Ph.D., of the Montefiore Einstein Center for Cancer Care in New York, one of many centers expected to participate in the trial that are also part of the NCI Community Oncology Research Program (NCORP).
Montefiore is an NCORP Minority Underserved site, meaning it serves a large population of racial/ethnic minorities or rural residents.
“So it’s a great place for answering questions about things like the impact of cost, health literacy … and all sorts of [screening] implementation issues,” said Dr. Rapkin, an NCORP investigator with the Montefiore program whose research focuses on the delivery of cancer care.
“One thing that’s going to be really important about the results of this trial,” Dr. Rapkin continued, “is translating the results in a way that can help people make informed decisions about screening.”


































No hay comentarios:
Publicar un comentario